THE DEFINITIVE GUIDE FOR THE TREATMENT OF DYSMENORRHOEA
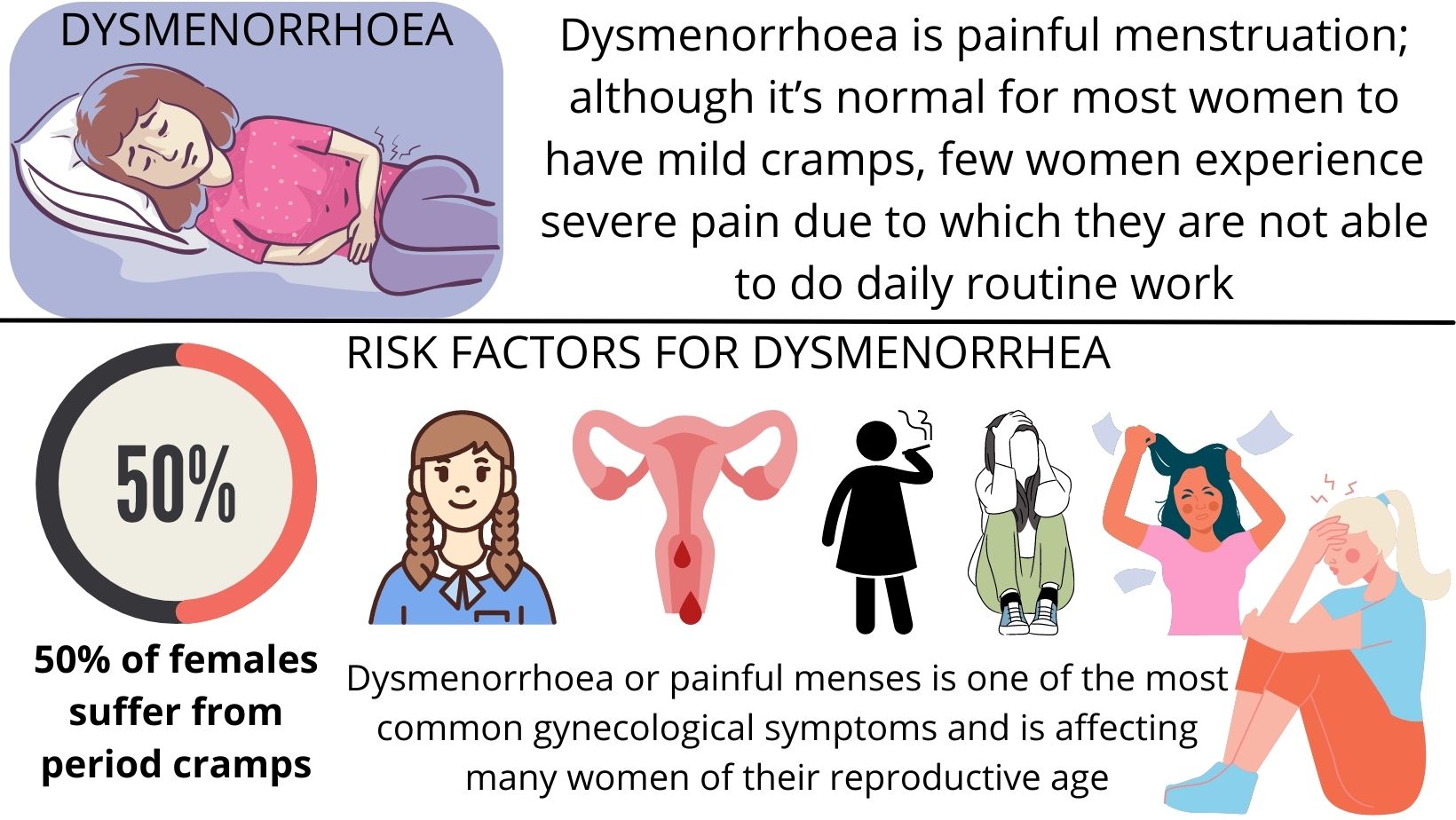
WHAT IS DYSMENORRHOEA?
Dysmenorrhoea is painful menstruation; although it’s normal for most women to have mild cramps, few women experience severe pain due to which they are not able to do daily routine work.
Dysmenorrhoea or painful menses is one of the most common gynecological symptoms and is affecting many women of their reproductive age.
WHAT ARE THE RISK FACTORS FOR DYSMENORRHEA
- Young age
- early menarche
- heavy menstrual flow
- nulliparity (a state in which a woman has never carried a pregnancy)
- smoking
- depression
- anxiety
- stress
WHAT ARE THE TYPES OF DYSMENORRHOEA?
PRIMARY (no pathology)- primary dysmenorrhoea is the presence of painful menses in absence of any pathology.
Primary dysmenorrhoea is caused by excessive levels of prostaglandins (hormones that cause contraction of the uterus). it affects adolescent girls but the problem ceases as they mature, particularly after a pregnancy.
Age at onset: 16–25 yrs
In primary dysmenorrhoea pain typically begins with the onset of menses and lasts for 12-72 hours. The pain is typically most severe on the first day and diminishes gradually.
Primary dysmenorrhoea is usually seen in absence of ovulatory cycles.
It usually begins within 6 to 12 months from the onset of menarche.
The pain is confined to the lower abdomen and is most intense in the midline which is crampy and intermittent.
Women often complain about pain in the back and thighs as well as nausea, diarrhea, headache, fatigue, malaise.
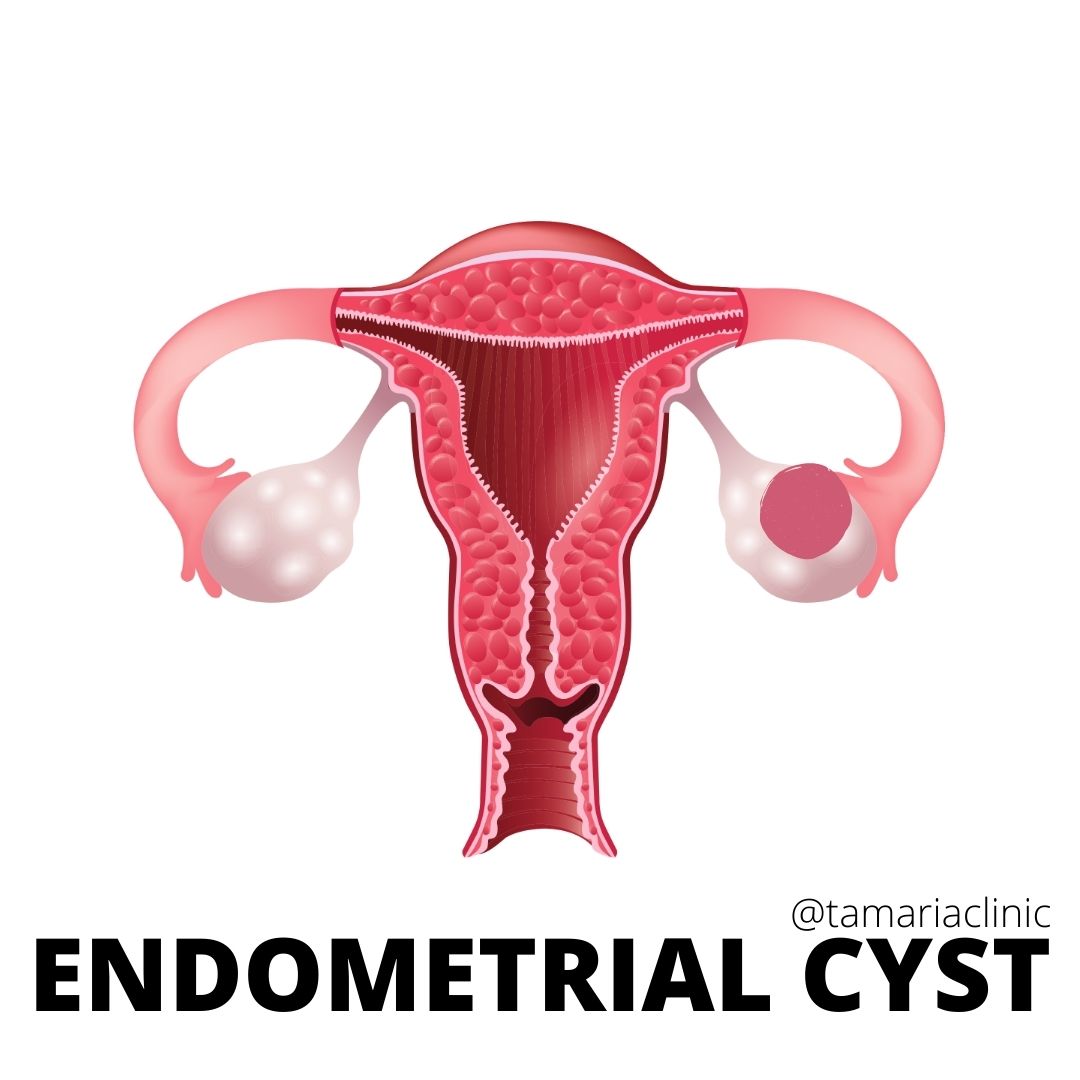
SECONDARY (related to some underlying gynecological disorder)- Dysmenorrhea is secondary when there is an identifiable anatomic or macroscopic pelvic pathological condition.
There may be associated
- vaginal discharge
- dyspareunia (painful sexual intercourse)
- menorrhagia (heavy bleeding at menstruation).
Secondary dysmenorrhoea is seen in conditions like
- fibroid
- adenomyosis
- sexually transmitted infection
- endometriosis
- pelvic inflammatory disease
- ovarian cyst
- intrauterine device.
It affects women in adulthood and most of the disorders can be treated easily.
Pain in secondary dysmenorrhoea (congestive) increases through the luteal phase (before the period starts) peaking at the onset of menstruation.
WHAT ARE THE SYMPTOMS OF DYSMENORRHOEA?
In primary dysmenorrhoea pain typically starts with the onset of menses and diminishes gradually. The pain is crampy, intermittent, and confined to the lower abdomen. The pain is often associated with pain in the lower back, thighs, diarrhea, nausea, vomiting, malaise, headache, fatigue.
In secondary dysmenorrhoea, pain is congestive and starts before menses which reaches to peak at the onset of menses. There may be associated vaginal discharge, dyspareunia (painful sexual intercourse), menorrhagia (heavy bleeding at menstruation).
WHAT ARE THE CAUSES OF DYSMENORRHOEA?
Primary dysmenorrhoea doesn’t have any underlying pathology except for high levels of prostaglandins.
For secondary dysmenorrhoea:
COMMON CAUSES
- Endometriosis
- Pelvic Inflammatory Disease ( Infections)
- Adenomyosis
- Intrauterine polyps
- Submucosal fibroids
- IUCDs
LESS COMMON
- Congenital uterine abnormalities
- Cervical stenosis
- Asherman syndrome
- Chronic ectopic pregnancy
- Pelvic congestion syndrome
- Ovarian cysts or neoplasms
DIAGNOSIS OF DYSMENORRHOEA
- History taking and physical examination along with pelvic examination would diagnose the case.
- A transvaginal ultrasound should be performed if secondary dysmenorrhoea is suspected.
TREATMENT OF DYSMENORRHOEA
Treatment of dysmenorrhea is aimed at providing symptomatic relief as well as inhibiting the underlying processes that cause symptoms.
Primary dysmenorrhea responds to
1.NSAIDs (nonsteroidal anti-inflammatory drugs, blocking the production of prostaglandins) that provide analgesic (pain-killing) and anti-inflammatory effects eg: aspirin, ibuprofen, and naproxen. Should be offered as a first-line treatment for pain relief.
2.COCs (combined oral contraceptives) are commonly used as second-line therapy when NSAIDs are ineffective, poorly tolerated, or contraindicated. COCs inhibit ovulation and endometrial tissue growth, thereby decreasing prostaglandin release. Contraception is the additional benefit of COCs.
Treatment of Secondary dysmenorrhea must address the underlying disease ( cyst removal/ removal of submucosal fibroids/polyps etc ). Secondary dysmenorrhea may be resistant to NSAIDs and COCs.
Homeopathic medicines would relieve the symptoms without any side effects and would give permanent relief as well.
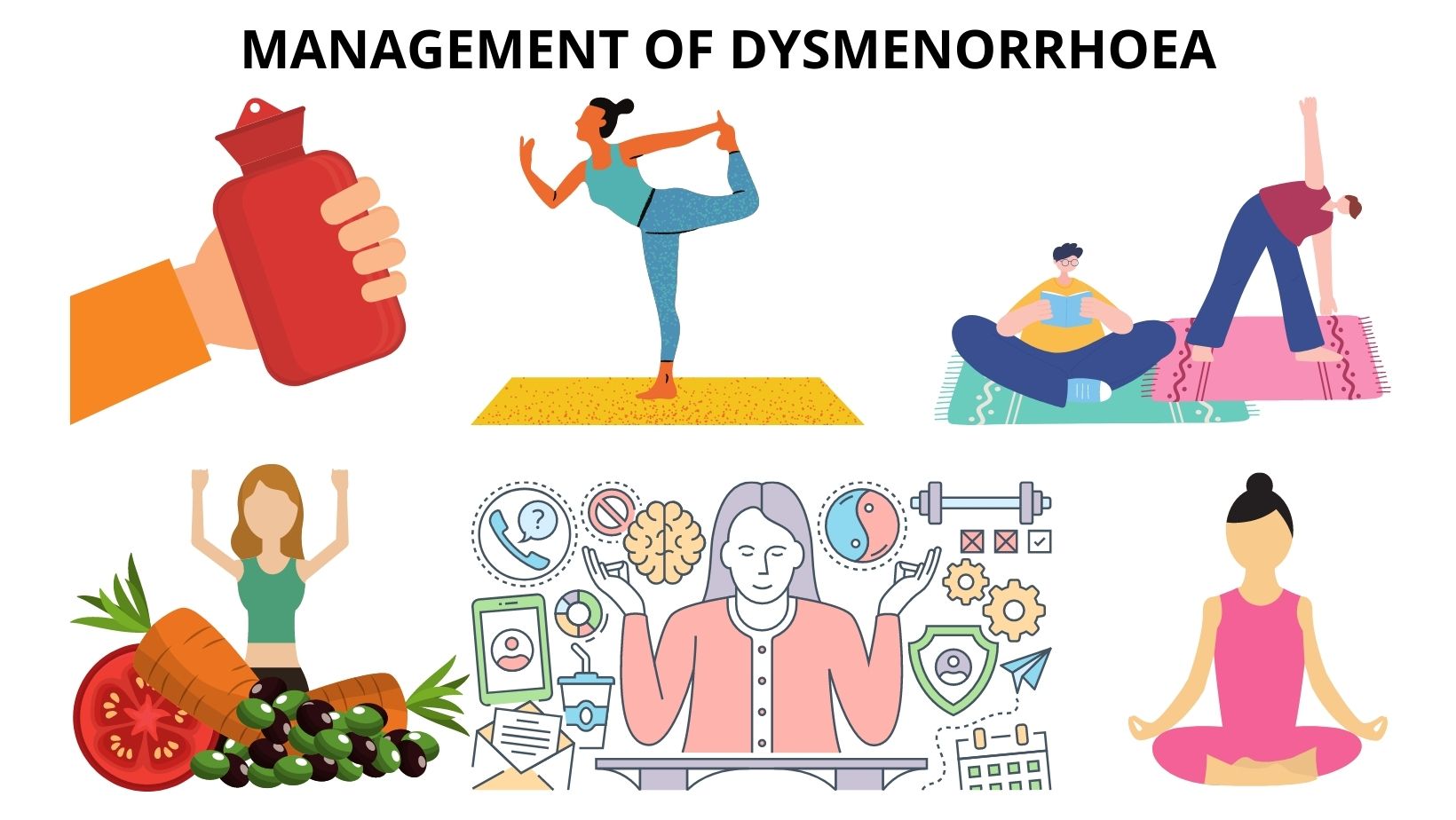
MANAGEMENT OF DYSMENORRHOEA
-
Pain management is very important.
-
Ask the patient to stay active and do regular physical exercise.
-
The patient should be advised to do yoga.
-
Advice patient to use a hot water bottle for fomentation during pain.
-
The patient should be advised to take a healthy diet.
HOMEOPATHIC MANAGEMENT OF DYSMENORRHOEA
Homeopathic medicines like mag phos, dioscorea, sepia, pulsatilla, sabina, graphites, colocynth, etc are a few medicines that are very effective in the treatment of dysmenorrhoea depending on the symptoms with which the patient presents.
DO’S AND DON’TS
DO’S
- Regular exercise.
- Yoga
- Healthy diet.
- Healthy lifestyle
DON’TS
- Manage anxiety/ stress
- Quit Smoking.
- Don't take Alcohol
Comments
We have received your comment , Thank You !